Medication Management of Antipsychotic-Induced Weight Gain in Children and Teens
Podcast, Volume , Number ,
https://www.thecarlatreport.com///
CME: Podcast CME Post-Tests are available using this subscription. If you have already enrolled in that program, please log in.
Published On: 07/25/2022 Duration: 13 minutes, 19 seconds Referenced Article: “Eating Disorders in Children and Adolescents ” The Carlat Child Psychiatry Report, July/August/September 2022 Joshua Feder, MD, and Mara Goverman, LCSW, have disclosed no relevant financial or other interests in any commercial companies pertaining to this educational activity Dr. Feder: Of approximately one million US children and adolescents, roughly 1% are prescribed second-generation antipsychotics. These medications routinely lead to weight gain in kids and teens even beyond the 7% that the FDA’s calls it’s ‘level of concern’. The worst offenders are olanzapine, quetiapine, and risperidone. Lurasidone and ziprasidone are of less concern, and of course there is every bit of in between including aripiprazole. In this episode, we’ll discuss the efficacy and safety of using off-label medications, such as metformin, to manage metabolic side effects of second-generation antipsychotics. Welcome to The Carlat Psychiatry Podcast. This is another episode from the child psychiatry team. I’m Dr. Josh Feder, The Editor-in-Chief of The Carlat Child Psychiatry Report and co-author of The Child Medication Fact Book for Psychiatric Practice and the brand-new book, Prescribing Psychotropics. Mara: And I’m Mara Goverman, a Licensed Clinical Social Worker in Southern California with a private practice. Dr. Feder: We have some exciting news for you! You can now receive CME credit for listening to this episode and all new episodes going forward on this feed. Follow the Podcast CME Subscription link in the show notes to get access to the CME post-test for this episode and future episodes. Mara: Let’s begin by talking about metformin, a medication approved for type II diabetes and it’s the best-studied treatment for metabolic side effects of second-generation antipsychotics. It functions by increasing insulin sensitivity in the liver and muscle and decreasing both hepatic glucose production and intestinal glucose absorption. The IMPACT study which measured the effects of metformin in children and adolescents on second-generation antipsychotics showed that while metformin stopped ongoing weight gain, it led to minimal weight loss and metabolic improvement over the course of the study. After 24 weeks, metformin patients lost 0.4 pounds, while control patients gained 8.5 pounds. These results sound encouraging, but what are the associated side effects of metformin? Dr. Feder: The most common side effect of metformin in the IMPACT study was mild to moderate gastrointestinal distress, with symptoms such as decreased appetite, abdominal pain, nausea and vomiting, diarrhea, and encopresis. Also, there are a lot of people who get gas. These symptoms occurred early, were mostly transient, and were manageable by slowing titration or using a lower dose of metformin. So, when is the best time to start metformin? Mara: Well, even though metformin can prevent future weight gain, it is unlikely to decrease existing weight. This means that if a child is already overweight for their height or if you are starting an antipsychotic with a high risk of weight gain, it is important to start metformin alongside the antipsychotic. If families resist starting two medications at once, check your patient’s height and weight, and start metformin if their weight begins to rise at a greater rate than expected, based on their growth. Dr. Feder: Before starting metformin, make sure to check the patient’s kidney function. Metformin is contraindicated if the GFR is <30, due to increased risk of lactic acidosis. It is safest to have a GFR above 60. Serum creatinine and serum B12 level should be checked annually if kidney function is normal meaning the eGFR is above 60, and more frequently if eGFR is between 45 to 60. If eGFR is less than 45, it is safest to stop metformin. When beginning metformin, make sure to titrate slowly to minimize gastrointestinal side effects. We recommend following the schedule used in the IMPACT trial. Here is the recommended dosage for youth based on weight. Mara: Topiramate is another medication that, similar to metformin, prevents weight gain better than it reduces weight. In a meta-analysis of randomized controlled trials of adjunctive topiramate for schizophrenia, 22 out of 26 trials showed topiramate led to a significantly lower body weight of 2.75 kg. An 11-week open trial in adolescents with medication-induced weight gain, titrated topiramate to 150 mg/day, giving a mean weight loss of 2.62 kg. In another meta-analysis of randomized controlled trials of topiramate in the treatment of obesity in adults, they found that, at doses of 96–200 mg/day, trials of less than 28 weeks led to a weight loss of 4.11 kg, and trials longer than 28 weeks led to a weight loss of 6.58 kg. Side effects of topiramate include oligohidrosis (decreased sweating) and hyperthermia during exercise, metabolic acidosis, word-finding problems, and cognitive impairment. Cognitive impairment may be avoided with a slow titration by 25 mg/week. Other side effects include a two- to four-fold increased risk of kidney stones, paresthesias, acute myopia with angle-closure glaucoma, and visual field defects. So, what is the best way to prescribe topiramate? Dr. Feder: Start topiramate at 25 mg per day, increasing by 25 mg every week as tolerated to a maximum dose of 150–200 mg/day. Higher doses are not more efficacious based on the minimal data available. Mara: Is the combination of metformin and topiramate safe or effective? Dr. Feder: Well, according to a recent case report of an 8-year-old with antipsychotic-associated weight gain the combination of metformin and topiramate was shown to be safe and effective. Zheng and colleagues (2016) also suggest considering combining metformin and topiramate when monotherapy is insufficient. However, since both metformin and topiramate can cause metabolic acidosis, make sure to check labs every few weeks until you reach steady dosages. Then recheck after dosage adjustments or significant weight loss, as significant weight loss also increases the relative dosage. Mara: Now, you may be tempted to use stimulants to prevent antipsychotic-associated weight gain, but in fact studies have shown lack of efficacy. Dr. Feder: And then there’s Lybalvi. Mara: This combination of olanzapine and samidorphan, which is an opioid antagonist, was recently approved to treat adults with bipolar disorder and schizophrenia and is purported to cause less weight gain; however, it has not been studied in children. Another medication researched for its use in antipsychotic weight gain is glucagon-like peptide, also known as GLP-1 agonists. GLP-1 agonists are almost all weekly injectable medications—with the exception of semaglutide (Rybelsus), which is used orally for adults with diabetes. They are FDA approved for use in type II diabetes and weight management. GLP-1 agonists decrease appetite, delay gastric emptying (which promotes satiety), and increase visceral and intra-organ lipolysis. For children and teens, liraglutide (Victoza, Saxenda) is approved for ages 10 and up for type II diabetes, and ages 12 and up for weight management. However, it is expensive. Saxenda costs $1,628/month retail, $1,315/month with GoodRx. Typical prior authorization criteria includes a BMI over 30 without comorbid conditions, or a BMI above 27 with comorbid conditions, and failure to lose 5% of body weight after three months in a weight loss program. Dr. Feder: GLP-1 agonists are contraindicated in patients with a history of pancreatitis, medullary thyroid cancer (including a family history), and multiple endocrine neoplasia type II. They should be used with caution in patients with renal insufficiency, and they can increase the risk of gallbladder disease. Despite the allure of GLP-1 agonists and although case studies report good effects in young teens with Prader-Willi syndrome, we do not yet have much data on their use in antipsychotic-associated weight gain. And boy it is expensive and hard to get. Ive tried and its really hard. Mara: Overall, when you need to use second-generation antipsychotics, consider starting with meds less likely to cause weight gain, such as lurasidone or ziprasidone. If you are using a different second-generation antipsychotic, think about starting metformin simultaneously, especially for patients with BMI >25. For patients with BMI >30, consider starting a GLP-1 agonist with the second-generation antipsychotic. Dr. Feder: The newsletter clinical update is available for subscribers to read in The Carlat Child Psychiatry Report. Hopefully, people will check it out. Subscribers get print issues in the mail and email notifications when new issues are available on the website. Subscriptions also come with full access to all the articles on the website and CME credits. Mara: And everything from Carlat Publishing is independently researched and produced. There’s no funding from the pharmaceutical industry. Dr. Feder: Yes, the newsletters and books we produce depend entirely on reader support. There are no ads and our authors don’t receive industry funding. That helps us to bring you unbiased information that you can trust. Mara: And don’t forget, you can now earn CME credits for listening to our podcasts. Just click the link in the description to access the CME post-test for this episode. As always, thanks for listening and have a great day!
Second-generation antipsychotics routinely breach the FDA’s level of concern of >7% body weight gain. This article examines the efficacy and safety of using off-label medications, such as metformin, to manage this side effect.
Interestingly, metformin was associated with fewer problems with aggression, hostility, anger, irritability, and impulsiveness. The authors of the study postulated this could be due to feeling less “hangry” or having better glucose homeostasis. Some of the rare potential side effects which were not observed in this study include low serum vitamin B12 level and metabolic acidosis. The only absolute contraindications to the use of metformin are chronic kidney disease and low glomerular filtration rate (GFR).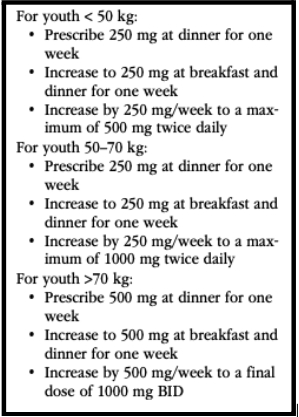




Leave A Comment
You must be logged in to post a comment.